What happens when a healthcare entity, institution, or partner unintentionally slips up (as in accidentally failing to) or neglects to comply with HIPAA regulations? The answer is simple — they're obligated to face hefty HIPAA violation penalties. But how costly can those penalties be? In this article, we'll discuss it in detail.
The Health Insurance Portability and Accountability Act (Act) 1996 was introduced by the U.S. Congress with one clear mission—to improve healthcare delivery, protect patient privacy, and safeguard the most sensitive piece of data, protected health information (PHI). But they didn't stop at framing the act; they took a step further and imposed hefty penalties for those who failed to comply with the rules.
Now, you might say, "Why is there even a need to impose penalties? After all, it's a legal requirement. Wouldn't entities already be motivated to adhere to the regulation?"
Sometimes, the law, let alone the law itself, is not enough to ensure everyone plays by the rules. Moreover, it's a general tendency; no one would put in the time, effort, and resources to comply with regulations if there were no consequences for neglecting them (you simply cannot bind them to do so).
That's why HIPAA penalties exist—not only to discourage wrong practices but also to ensure that every healthcare entity/institution and its partners take their responsibilities seriously and remain committed to safeguarding PHI.
Note: HIPAA compliance applies to healthcare clearinghouses, healthcare providers, Medicare prescription drug card sponsors, and business associates (which include individuals or entities that handle PHI). Therefore, if any of these parties violate HIPAA, they are liable to face the corresponding consequences.
Now, let's dive deeper and explore the penalties for HIPAA violations.
HIPAA Violation Penalties: A Category-Wise Breakdown
Before we discuss the penalties in detail, let’s ask one important question: ‘Are all healthcare providers (the ones who violate compliance) subject to the same penalties?’
The answer is – NO! Organizations are penalized only based on the severity and intent behind the offense. But why aren’t they penalized the same way? After all, they are violating the law in the end.
Let’s break it down: some healthcare organizations might unintentionally fail to comply, perhaps due to an oversight or misunderstanding. On the other hand, there are those who deliberately choose to ignore compliance. Then, there are those who willingly engage in wrongful practices and are fully aware of the consequences. Clearly, these actions aren’t all the same, so how can penalties be applied?
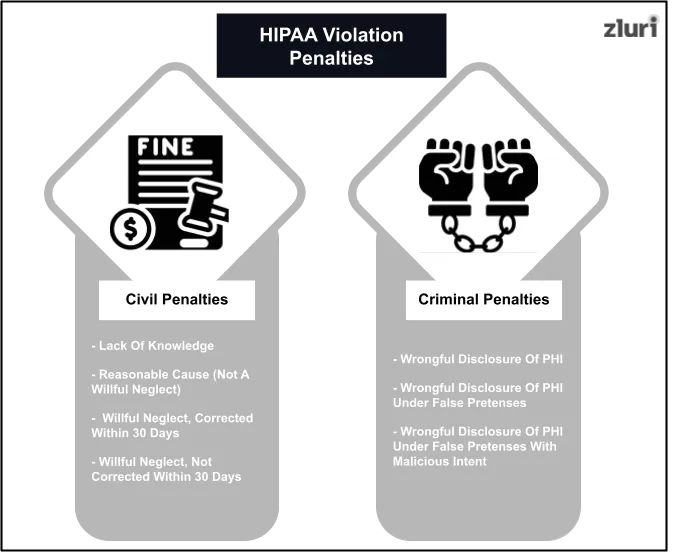
In fact, to ensure that penalties are proportionate to the nature of the offense, HHS (US Department of Health and Human Services) and the OCR (Office of Civil Rights) even classified HIPAA violation penalties into two main categories: civil HIPAA violation penalties and criminal HIPAA violation penalties. Each category is further divided into graded tiers.
Note: The mentioned HIPAA violation penalties are in accordance with the latest figures released on August 8, 2024 (these fines are adjusted for inflation). These rates (civil Monterey HIPAA violation penalties) will be enforced for violations that occurred on or after November 2, 2015, regardless of when the HIPAA violations are assessed. The 2024 rates will remain in effect until the HHS publishes a final rule in the Federal Register to adjust the penalty amounts for inflation in 2025.
Category 1: Civil HIPAA Violation Penalties
Category 2: Criminal HIPAA Violation Penalties
Note: The OCR handles civil Monterey HIPAA violation penalties, and the DOJ (Department of Justice) takes charge of criminal penalties (which involve monetary fines and jail time).
Factors Impacting The Imposition Of HIPAA Violation Penalties
Besides considering severity and intent, OCR and DOJ also consider the factors listed below when penalizing healthcare providers, entities, or their partners who have committed the felony (as in violated HIPAA compliance).
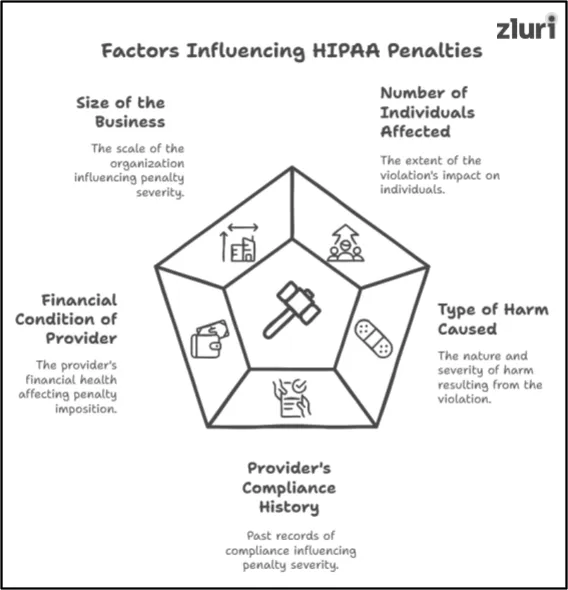
Factor 1# The Number Of Individuals Affected: OCR and DOJ evaluate how many individuals were affected by the violation. If the numbers are high, the HIPAA violation penalties will also be high. Basically, the wider the reach of the violation, the more serious the consequences.
Factor 2# The Type Of Harm caused: The regulatory authorities assess whether the violation caused physical, financial, or reputational damage or perhaps hindered a patient's ability to access healthcare services, and based on the findings, they impose appropriate HIPAA violation penalties.
Factor 3# The Provider's Compliance History: The regulatory authorities carefully review a healthcare provider's compliance history (past records of compliance). If the providers have a past history of non-compliance, they will be charged higher HIPAA violation penalties, as their actions demonstrate a recurring pattern of negligence. Meanwhile, a clear compliance record might reduce the penalty charges.
Factor 4# The Financial Condition Of The Provider: The regulatory authorities also consider the provider's financial health before imposing any HIPAA violation penalties. They make sure that the penalty is not so severe that it could further impact the provider's ability to continue operating and providing care to patients (as in, the risk of shutting down).
Factor 5# Size Of The Business: The regulatory authorities imposed high HIPAA violation penalties for larger practices. This is because if a larger organization violates HIPAA compliance, it will expose more PHI, impacting more individuals. Meanwhile, the authorities imposed lower HIPAA violation penalties for smaller organizations because they recognize that smaller practices lack the financial strength to bear severe fines.
After going through the factors, you will probably be curious about which actions are considered HIPAA violations. So, let's quickly explore the examples of HIPAA violations.
Common Examples of HIPAA Violations
Listed below are the actions that are considered HIPAA violations.
- Accessing PHI or other health care records without authorized permission.
- Denying to provide patients access to their medical records.
- Not encrypting ePHI or not implementing necessary security measures to safeguard ePHI.
- Disposing of PHI improperly.
- Downloading PHI on unapproved or unauthorized devices.
- Sending ePHI to personal email accounts.
- If a data breach occurs (where the PHI is compromised), the organization must notify affected individuals and the Department of Health and Human Services (HHS) within 60 days of discovering the breach. Exceeding the 60-day deadline is considered a violation.
- Disclosing PHI after authorization expiry.
Now that you know the HIPAA violation penalties, let’s address one common question — ‘How are these violations discovered? After all, no one will confess to the felony they committed.’ To find the answer, read on.
How OCR & DOJ Discover HIPAA Violations?
OCR and DOJ rely on two primary sources to detect HIPAA violations:
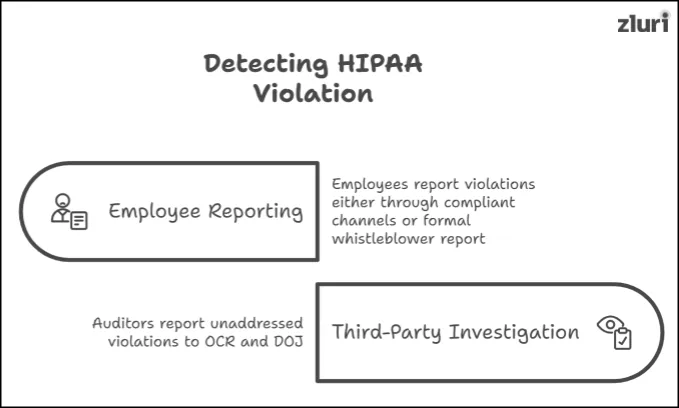
- Employee Reporting: When employees discover that their colleague or their organization is violating HIPAA rules, they typically report it to the OCR and DOJ—either through formal whistleblower reports or other complaints channels.
- Third-Party Investigation: Organizations often bring in an external certified auditor to perform an audit and issue certification to obtain HIPAA compliance certification. So, when the external auditor detects any violation during the audit process, they generally request the organization to make the corrections. However, if the organization deliberately neglects to take corrective action after being requested to do so, the external auditor escalates the matter and files a violation complaint with the OCR and DOJ.
However, OCR and DOJ don't rely solely on the reports they receive from employee whistleblowers and third-party investigations. They also proactively conduct random audits (particularly targeting organizations that may show signs of suspicious activity or non-compliance) to discover HIPAA violations.
Violating HIPAA Can Cost You Far More Than Just Monetary Penalties
Most organizations have a common misconception — they believe that if they violate HIPAA compliance, they will only incur monetary fines (HIPAA violation penalties) or serve prison time. Well, that's not entirely true. The actual consequence of a HIPAA violation is far more than just monetary penalties and imprisonment. A violation can severely damage your business reputation. How? When an organization fails to demonstrate its commitment to securing the PHI (violating HIPAA), it sends a clear message to investors, clients, and partners—that they don't take security seriously. This perception destroys trust and confidence, turning you from a reliable business into one seen as reckless and unreliable (completely running your credibility in the market). And once your reputation is tarnished, rebuilding it will cost more than any fine you could pay.
Now, after discovering the severe repercussions, you might be eager to know how to avoid violating HIPAA. (Let's be real: After learning about the fallout, you'll want to stay on the right side of compliance).It's simple—you just have to follow this HIPAA compliance checklist (click to find out what is included in the checklist), avoid engaging in wrongful practices (misconduct), and perform reviews periodically.
Also Read: How to Perform Periodic User Access Review?
Note that you can hire external auditors (which can be expensive) or use tools like Zluri's access review solution (a more economical option) to perform the review. The platform is designed to simplify the user access reviewing process.
Also Read: 6 Best Approaches to Perform an Effective User Access Review
Here's how it works: It provides your team (the reviewing team) with all the insights required from reviewing in one single place (be it application data or user data), eliminating the need to scroll through directories and spreadsheets to gather data. Your team can review the data and take spot-on (without having to switch tabs) remediation measures.
Lastly, it generates a detailed user access review report outlining all the actions performed during the review. You can further directly present these reports as proof of evidence to external auditors (who are certified to issue compliance certification) and obtain compliance certification successfully.
Also Read: Penalties For SOX Violation







.svg)














